St. Mungo's Hospital
Hospitalist History and Phyiscal Exam
Acute Care Setting (Setting 1)
NAME: James Krum
MRN: H07311980
AGE: 64 year old DOB: 12/25/1960
PRIMARY CARE PROVIDER: Dr. Horace Lovegood
REASON FOR ADMISSION: CVA (cerebral vascular accident) (*)
HISTORY OF PRESENT ILLNESS: Patient is a very pleasant 64 year old male with a past medical history as noted below. Patient presented to hospital today from primary care clinic for suspected stroke. About last Wednesday evening around 9 PM (it is now the following Monday afternoon), he noticed that he dropped a glass out of his left hand. He noticed some continued mild left hand weakness since then, but on Saturday there was an episode where his whole left arm essentially became numb and paralyzed. Since that time, he noticed some improvements in the weakness, but the numbness has not completely resolved. He has had a feeling of being slightly off balance and has had a couple of falls since then. He has chronic sinus congestion and he thought the falls may have been related to that. He also reports a right sided headache for the last few days, but he is unsure of the onset and if it correlates with the onset of his symptoms of weakness and numbness last Wednesday. He has not taken his Aspirin for about 1 month since he ran out. His son had noted that his speech was a bit slurred. Patient states that he didn't think that his symptoms were "a big deal", so that is why he delayed medical care.
In the ED, patient was seen and evaluated. Initial vital signs at 1535 were as follows:
·Temp: 98.5 °F (36.9 °C) oral
·Heart Rate: 93
·Resp: 18
·BP: 120/71 mmHg
·SpO2: 95 %
Labs and imaging also completed in the ED. Neurology consulted. Patient was given a full strength Aspirin and 300 mg of Plavix.
PAST MEDICAL HISTORY:
·Chronic bilateral knee pain – 2018
· Concussion – several in lifetime dating back to 1990
· Coronary Artery Disease – 2012
·Depression – 2004
·Diabetic retinopathy – 2023
·Hyperlipidemia – 2012
·Hypertension – 2012
·Transient Ischemic Attack – 2021
·Type II Diabetes Mellitus – 2012
PAST SURGICAL HISTORY:
· Cardiac catheterization – 2012 and 2013
o Total of 2 stents in 2012, 1 stent in 2013
· Excision of lesion, back or flank – 2018
o Lipoma upper right back, 10 cm
·Shoulder arthroscopy – 2021
o Left shoulder arthroscopy, arthroscopic subacromial decompression, mumford, labral debridement, paralabral cyst excision, and biceps tenotomy
CURRENT MEDICATIONS:
Prescriptions Prior to Admission
·Aspirin – 81 mg twice daily
· Atorvastatin – 40 mg daily
· Ezetimibe – 10 mg daily
· Furosemide – 20 mg daily
· Insulin glargine – 300 mL/unit, 22 units daily
· Jardiance – 25 mg daily
· Losartan – 50 mg daily
·Metformin – 2000 mg daily
· Metroprolol tartrate – 25 mg
·Omega-3 fatty acid – 1000 mg
FAMILY HISTORY:
· Diabetes – Mother, onset 55 years
· Heart/vascular – Mother, onset 68 years
· Stroke – Paternal Grandfather, onset 75 years
· Cancer (breast) – Sister
Remainder of patient's family history is not pertinent to this hospitalization.
REVIEW OF SYSTEMS:
· Constitutional: Negative.
· HENT: Negative.
· Eyes: Negative.
· Respiratory: Negative.
· Cardiovascular: Negative.
· Gastrointestinal: Positive for nausea.
· Genitourinary: Negative.
· Musculoskeletal: Negative.
· Skin: Negative.
· Neurological: Positive for dizziness and weakness.
· Psychiatric/Behavioral: Negative.
All other systems reviewed and unremarkable.
PHYSICAL EXAM:
Vital signs at admission as of 1745
· Temp: 98.5 °F oral
· Heart rate: 85 bpm
· Respiratory rate: 18 breaths/minute
· BP: 183/103 mmHg
· SpO2: 95%
· Height: 1.727 m (5’8”)
· Weight: 108.2 kg (238 lb 9.6 oz)
· BMI: 36.28 kg/ m²
Physical Exam
· Constitutional
o General: no acute distress
o Appearance: normal appearance, non-toxic appearing
· Head/ear/nose/throat
o Head: normocephalic and atraumatic
o Mouth: Mucous membranes are moist
· Eyes
o Pupils: equal, round, and reactive to light
o Extraocular movements: normal and intact
· Cardiovascular
o Rate and rhythm: normal rate and regular rhythm
o Pulses: normal pulses
o Heart sounds: normal heart sounds
· Pulmonary
o Effort: normal
o Breath sounds: normal
· Abdominal
o Palpations: abdomen is soft
·Musculoskeletal
o General: normal range of motion
o Cervical spine: normal range of motion
· Skin
o General: skin is warm and dry
· Neurological
o Mental status: alert and oriented x 4
o Sensory: no sensory deficit
o Motor: weakness present
o Coordination: finger-nose-finger test abnormal, heel to shin test normal
o Comments: NIH score of 3 due to left arm and leg drift and limb ataxia
· Psychiatric
o Mood and affect: mood normal
o Behavior: normal
o Thought content: normal
o Judgment: normal
LABS AT ADMISSION:
Complete Blood Count Without Differential – collection time 10/2/24 1521
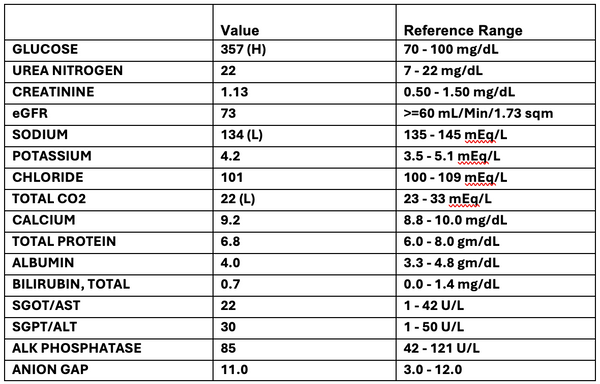
Comprehensive Metabolic Panel – collection time 10/2/24 1521
Other Lab Values – collection time 10/2/24 1521
ORDERS PLACED THIS ENCOUNTER:
·ECG – Adult/Pediatric – Standard 12 lead
·Imaging
o CT Head without Contrast
o CT Angio with Perfusion
o CT Angio Neck
·Consult Neurology
·Consult Physical Therapy/Occupational Therapy
ASSESSMENT:
·Acute hospital problem – left hand/arm weakness secondary to probable cerebral vascular accident, likely due to poorly controlled type 2 diabetes and hypertension.
o Positive history of TIA in June of 2021. Per electronic health record, CT was negative and head MRI and head/neck MRA did not show a discrete source of symptoms.
o Vital signs show elevated blood pressure with highest reading of 183/103 mmHg.
o ECG – normal sinus rhythm
o CBC and CMP unremarkable other than hyperglycemia. Repeat lab work tomorrow AM, including HgbA1c, TSH, and lipid panel.
o Head CT in ED – nonspecific white matter change and cerebral atrophy with findings in the right corona radiata most likely related to progressive vascular disease.
o Head/neck CT angio in ED – total volume of ischemia in the right MCA territory of 61 cc using a threshold of Tmax greater than 6 seconds, but there is no vascular stenosis or occlusion identified.
o Neurology consult in ED – patient not a candidate for tPA or neurointervention as he is outside the time window. Recommend patient be given 325 mg of aspirin x 1 and Plavix 300 mg x 1 followed by 81 aspirin mg daily and 75 mg Plavix daily for 3 weeks. Also recommend high-dose statin therapy. Long-term antiplatelet therapy to determine based on the results of these test
·Chronic conditions
o Type 2 Diabetes – poorly controlled, hemoglobin A1c in September was 8.8. Will continue home basal insulin at 20% decrease in home dose and monitor blood sugars with sensitive dose sliding scale insulin addition.
o Hypertension – will continue home medications with as needed labetalol, may need some adjustments in his home medications.
TREATMENT PLAN:
·MRI and Transthoracic Echo in AM
·Increase statin to 80 mg daily
·Will give labetolol prn for elevated blood pressure
·Bedside swallow screen by nursing – if pass then may resume diabetic diet
·325 mg Aspirin x 1 and 300 mg Plavix x 1, followed by daily aspirin 81 mg and Plavix 75 mg for 3 weeks minimum
·Consult physical and occupational therapies
·Consult neurology
·DVT Prophylaxis: SCDs
Code status: full
Disposition: anticipate < 2 midnights due to CVA
Thank you for the opportunity to participate in this patients care.
Time spent was 60 minutes on the behalf of this patient, with greater than 50% of the time spent in counseling and coordination of care, interviewing and examining patient, reviewing charts/labs/ radiology, and discussing diagnoses and treatment plan with patient, family, and medical staff.
Electronically signed by Remus Dursley, MD 10/2/2024 6:12 PM CST